What is PUJ obstruction?
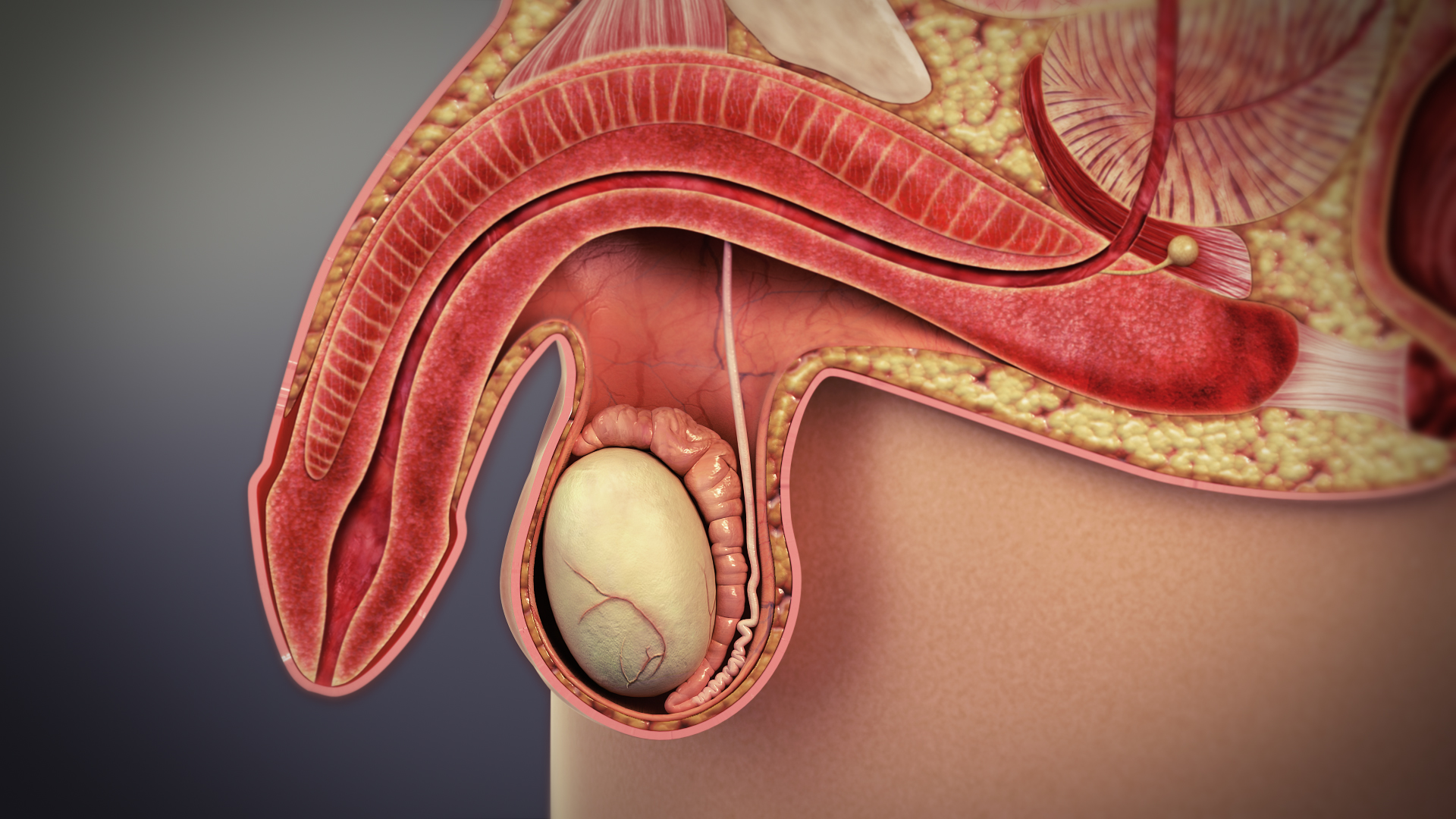
PUJ obstruction results from narrowing of the junction between the pelvis of the kidney and ureter, resulting in impedance to the flow of the urine from the kidney to the ureter.
The condition affects approximately one person in every 1000 adults and tends to occur more in men.
Most people have two kidneys, that filter the blood to remove waste products, which they excrete into the urine. Urine is carried from each kidney, through the ureter, to the bladder where it is stored.
As well as removing waste products, the kidney performs many vital functions, such as controlling fluid balance (how to dilute the blood is), regulating various salts or electrolytes in the bloodstream (eg: sodium, potassium, calcium, magnesium), maintaining the correct acidity of the blood, and regulating blood pressure.
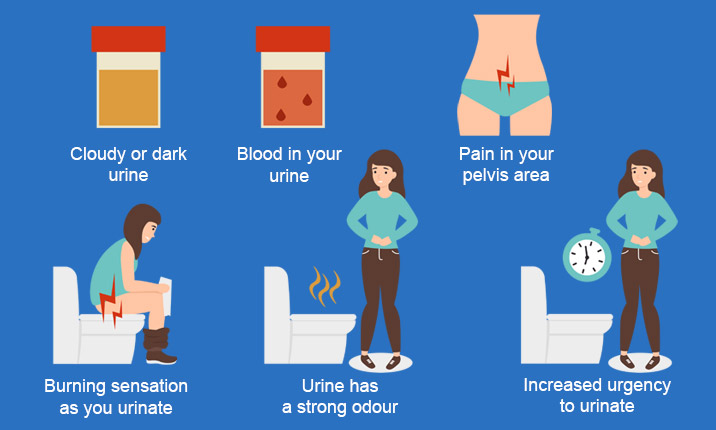
Many different conditions can affect the kidney; one of which is PUJ obstruction that causes no symptoms or problems and is only discovered by chance when the patient is having a scan for another condition. Alternatively, it can cause:
• Recurrent episodes of loin pain which tends to worsen after drinking especially alcohol.
• Kidney infection (pyelonephritis).
• Kidney stones.
• Lump or swelling in the kidney area.
• Damage to the kidney as a result of either high pressure in the renal pelvis, kidney infection, or formation of kidney stones.
How is Diagnosis of PUJ Obstruction?
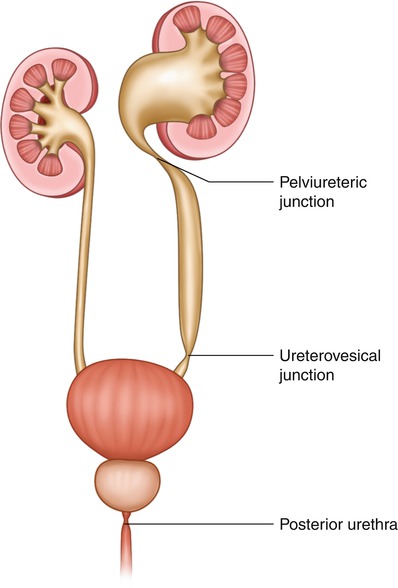
This includes blood tests, urine test,s and scans. CT scan is commonly used to assess the anatomy and the structure of the renal pelvis and a special nuclear medicine scan called MAG3 scan is used to confirm the obstruction and also to assess the function of the kidney.
If there is severe kidney infection as a result of the obstruction, then the kidney must be drained as a matter of urgency with insertion of a temporary ureteric stent or nephrostomy tube before any definitive treatment.
There are several treatment options for PUJ obstruction and these will be discussed with you; these include:
Active surveillance with careful observation with repeated scans.
Treatments for PUJ obstruction
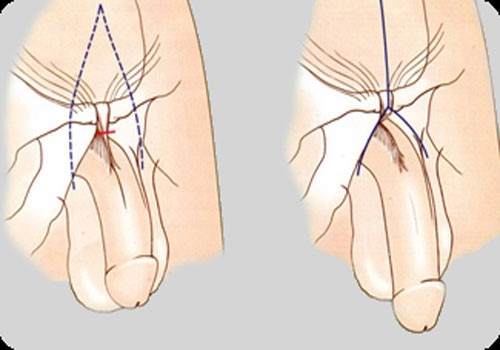
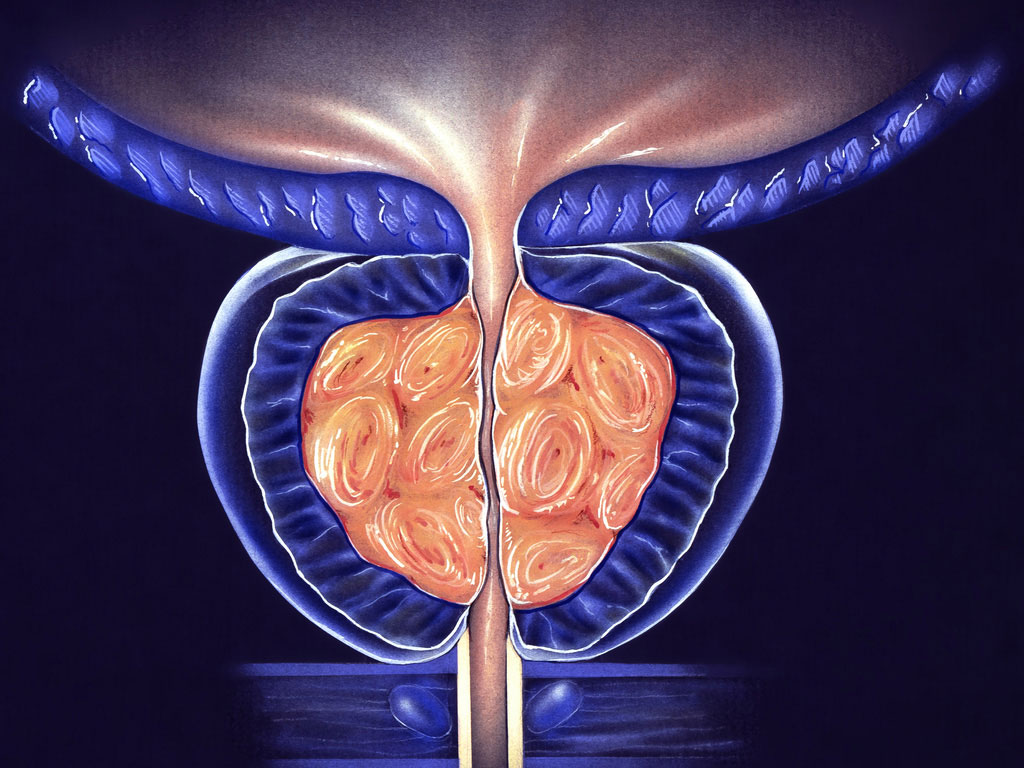
The PUJ is the portion of the collecting system that connects the renal pelvis to the ureter. The standard treatment for pelvic ureteric junction obstruction is pyeloplasty.
There are different ways to approach the kidney to perform the operation. These include via a flank incision, subcostal (under the rib) incision, transabdominal approach, or even sometimes through an incision in the back.
Most commonly, however, this procedure is done using laparoscopy, or keyhole surgery.
Laparoscopy is a technique of performing a surgical operation using instruments inserted through narrow hollow tubes (‘ports’) rather than through a larger incision, as in traditional surgery.
The result is shorter hospitalization and convalescence, often less bleeding and post-operative pain, and fewer wound complications.
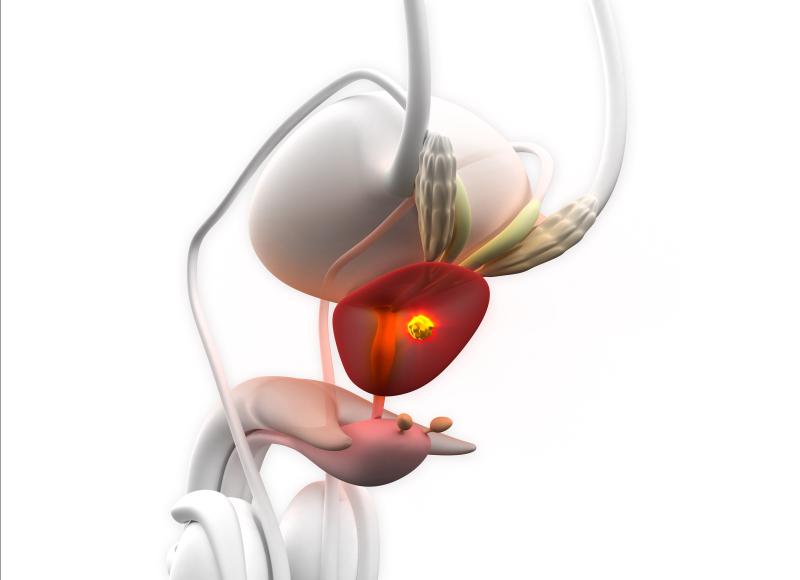
Chronic prostatitis Symptoms
There’s a reason behind naming chronic prostatitis as chronic pelvic pain syndrome. This is usually due to the vague presentation and different manifestations in different men. This could be ranging in the form of penile tip pain or scrotal discomfort. Others could present with chronic low back pain and pain during ejaculation. This could be well associated with storage lower urinary tract symptoms.