Once a stone former. always a stone former!!
Urinary tract stones are the most common encounters in the field of urology. “Doctor, I’d rather give birth to 10 children than going through the pain of passing a stone!” Says many of my female stone patients.
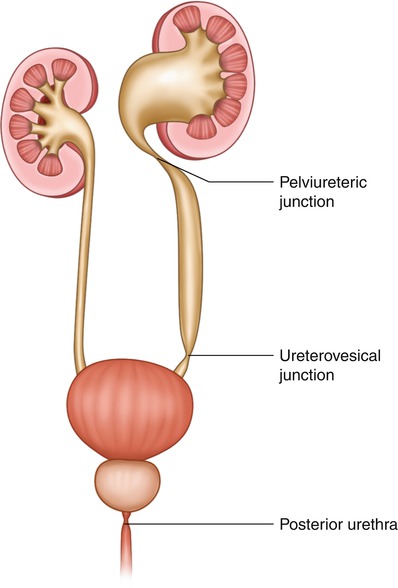
Ureteric colic is an uninvited guest that barges in at any time. It is so severe at times that pilots, divers, and those operating heavy machinery, when suffering from a ureteric stone, aren’t allowed to resume their work until the stone has passed, for the fear of their lives and others.
Prevention is better than cure, and there are many, inexpensive and easily adaptable lifestyle modifications that wild help minimizing the chances of stone recurrence rate.
Below are some advice Preventing the Stone Formation
Water
60% of our bodies are made of it. It makes absolute sense to maintain a healthy water intake.
Drinking plenty of fluid is the most effective way of preventing the stone formation and reduces your risk of stone formation by almost one-third (30 to 40%). Not drinking enough can cause your urine to become concentrated, making stones more likely to form.
Try to drink two to three liters (four to six pints) of fluid (water or squash) each day. You should aim to keep your urine colourless throughout the day. This should give you a urine output of at least two liters (four pints)per day.
What about other fluids?
I, like many people, am addicted to caffeine. Whilst it has some benefits, it has its implications in stone formation, mainly increasing the Oxalate component of stones. Not to mention the fact that these fluids would actually deprive the body of water due to their diuretic effects.
Kidney Stone Diet Tips that may help:
- Drink a large glass of water at specific times each day (e.g. when you get up, when you arrive at work, after using the toilet, etc);
- Keep a bottle or jug of water by your side all day; you can flavour it with fruit squash;
- Try to drink one glass of water every hour;
- Add slices of lemon, lime or orange to cold water; this gives it a pleasant flavour and helps to make your urine less acidic;
- Eat more fruit & vegetables because they contain a lot of water. Finally
- Include moist/liquid foods in your diet (e.g. soup, stew & jelly).
Calcium:
Opposite to the traditional belief, reducing the amount of calcium in your diet can increase the risk of stone formation, by raising oxalate levels in your urine. A daily intake of up to 1000 mg per day is safe for calcium stone formers.
Most dietary calcium is found in dairy products (milk, yogurt, cream and cheese). A normal, varied diet will give you about 500 mg of calcium each day. The approximate calcium contents of dairy produce are:
• milk and yoghurt – 120 mg per 100 g
• soft cheese – 400 mg per 100 g
• hard cheeses – up to 1000 mg per 100 g
They were the numbers that will hopefully help you identify the right quantity of dairy products for daily consumption
If you have too much calcium excreted in your urine, the restriction might be of benefit here, but better consult your doctor
What about the other culprit? Oxalate
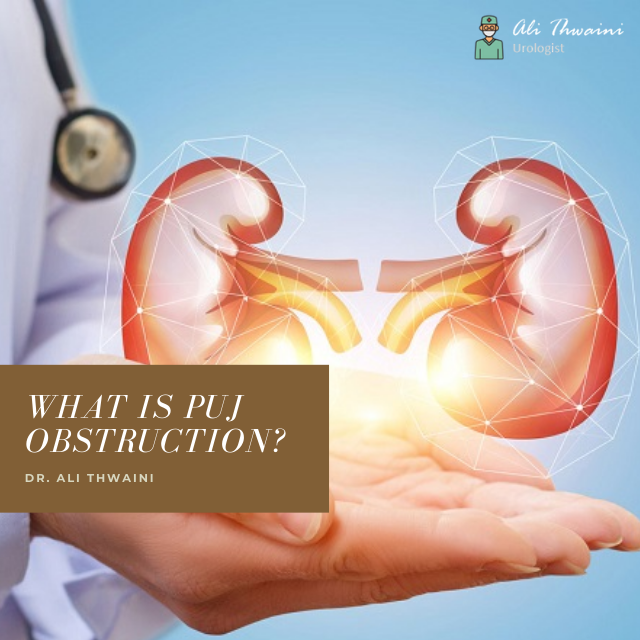
The majority of urinary tract stones are composed of calcium and oxalate. The latter is present and vast quantities of the following food items:
rhubarb, celery, spinach, beetroot and sesame seeds, all of which have large amounts of oxalate in them.
Black tea, chocolate, nuts (including peanut butter), cocoa and carob are all moderately high in oxalate.
Eating those items in moderation is the recommendation as most of them have lots of beneficial nutritional items.
Uric Acid Stones.
These are the second most common type of kidney stones. Historically they are related to large amounts of red meat consumption that could lead to gout, Hence the name Kings’ disease.
In addition to red meat the following items contain a large amount of uric acid and are butter taken in moderation by normal people and then matchless amounts by uric acid stone farmers:
• meat – all meats, including liver, heart, kidney, sweetbreads & meat extracts (e.g. Oxo)
• fish – especially anchovies, crab, fish roe, herring, mackerel, sardines, shrimps & whitebait
• others – yeast extracts (e.g. Bovril), beer, asparagus, cauliflower, mushrooms, peas, beans & spinach.
In summary
Urinary tract stones are one of the most common presentations and Urology and emergency. Stone attacks are very painful and cuddly to potentially serious illness and lots of work and activity.
Prevention is better than cure. Modification of lifestyle has amends beneficial results. For any further information and treatment visit your local urologist for further information and advice