UTIs during pregnancy are not uncommon and increase the risk of developing pyelonephritis, which is associated with an increased risk of fetal loss, premature delivery, and low birth weight babies. Screening can reduce the risk of this.
All women should be screened for asymptomatic bacteriuria at the 1st antenatal appointment
Symptomatic bacteriuria occurs in 17-20% of pregnancies. There are pathophysiological grounds to support a link to pre-labour,
premature rupture of membranes (PROM) and pre-term labour. Untreated upper UTI in pregnancy also carries risks of morbidity and rarely mortality to the pregnant women
Physiological changes in the pregnant woman make her more likely to suffer both asymptomatic bacteriuria (AB), and urinary infection (cystitis, pyelonephritis).
2-9% of women are bacteriuric in the first trimester. 10-30% of women with bacteriuria in the first trimester develop upper urinary tract infection in the second or third trimester
High fever, whether caused by UTI or other infection, is associated with foetal loss, at any stage in pregnancy.
Benefits of screening for asymptomatic bacteriuria:
Early screening for and treatment of asymptomatic bacteriuria in pregnancy has maternal and foetal benefits.
A Cochrane review of 14 randomized trials of asymptomatic bacteriuria in pregnant women compared the antibacterial therapy to that with placebo or no treatment. The Cochrane review showed that antibacterial therapy was significantly more likely to clear asymptomatic bacteriuria, to lower the incidence of pyelonephritis, and to reduce the rate of preterm delivery or low birth weight babies.
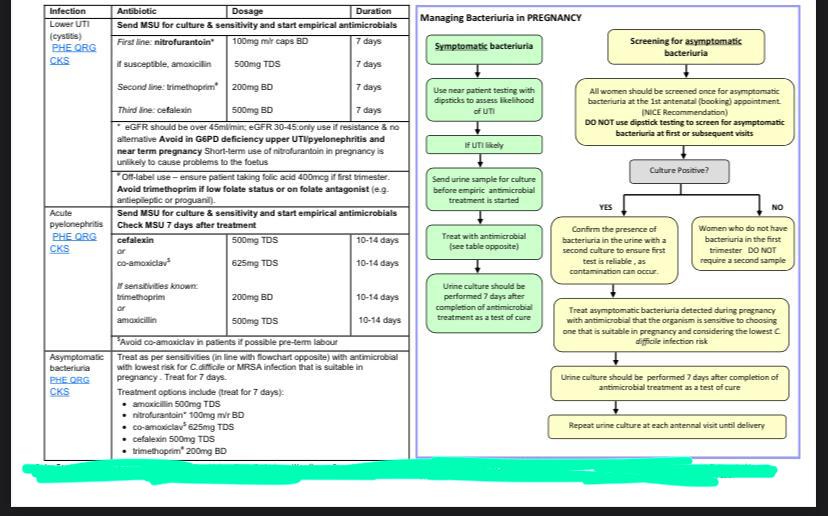
Screening for asymptomatic bacteriuria in pregnancy
All women should be screened once for asymptomatic bacteriuria at the
1st antenatal (booking) appointment (NICE recommendation).
Do this by sending an MSU. DO NOT USE DIPSTICKS: they are not sufficiently sensitive.
If positive result, repeat as indicated in the flow chart over the page to ensure first test is reliable , as contamination can occur.
Managing symptomatic bacteriuria
Symptomatic bacteriuria in pregnancy should be treated (see over page for guidance on antimicrobials).
Use near-patient testing with dipsticks to assess the likelihood of UTI. Send urine for culture before starting empirical therapy. Send a repeat sample 7 days after completing treatment as a test of cure.
Antimicrobials for bacteriuria in pregnancy
The choice of antibacterial and the duration of therapy depend on a number of considerations:
- The relative contraindications to some antimicrobials in pregnant women (always refer to the BNF)
- Resistance of the organisms;
- Adverse effect profiles (including propensity to cause C. difficile-
- infection).
- Use MSU results, when available, to guide therapy even if this entails a change of empirical therapy.
- Since most antimicrobials are concentrated in urine, oral therapy is sufficient in most patients
Managing incidentally-found group B streptococcus infection in urine
The antenatal care service should be informed when a group B streptococcus (GBS), Streptococcus agalactiae, is isolated in urine. Women with GBS bacteriuria identified during the current pregnancy should be offered IV antimicrobial prophylaxis during delivery .
GBS bacteriuria, is associated with a higher risk of choriamnitis and neonatal disease. However, it is currently not possible to accurately quantify these increased risks.
Women with GBS urinary tract infection during pregnancy should also receive appropriate treatment at the time of diagnosis as well as IV prophylactic antimicrobials as the time of delivery. Treatment of GBS UTI during pregnancy should be treated as per culture sensitivities. Refer to BNF for further advice on appropriate antimicrobials during pregnancy.
Urine Sampling
The specimen should be mid-stream. Cleansing with water and holding the labia apart are not essential. Use of antiseptics for cleaning the perineum is not
recommended as this can cause false negative culture results. Refrigerate specimens to prevent bacterial overgrowth.
Interpreting a culture result:
The following usually indicates UTI in a patient with urinary symptoms. Higher counts have even higher positive predictive values:
- Single organisms ≥ 104 colony forming units (CFUs)/ mL
- Mixed growths’ indicates perineal contamination which reduces the significance of the culture. If a culture is still required, an MSU should be repeated with patient counselled on correct sampling technique
- Culture results should be interpreted in the light of near-patient dipstick testing.
Microscopy:
Microscopy is not available for the diagnosis of UTI except in children <3years to comply with NICE guidelines. Use near-patient testing with dipsticks to assess the likelihood of UTI, they are as sensitive and specific as microscopy for predicting the presence of infection. Urine microscopy is only performed for? glomerulonephritis, SLE, endocarditis, haematuria, casts, crystals, candiduria and Schistosomiasis and must be specifically requested with the relevant clinical details.
Treatment: please refer to the following chart: