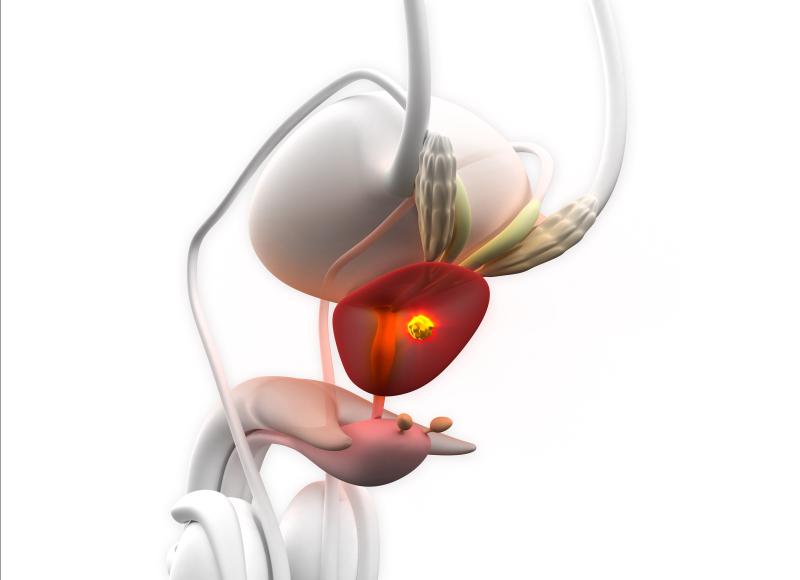
Lower urinary tract symptoms (LUTS) are complaints related to altered function of the urinary tract, and these include frequency (defined as the need to pass urine very often); urgency (the need to pass urine without much warning); urge incontinence (urgency resulting in leakage of urine which you cannot control); hesitancy (not being able to pass urine immediately); poor flow ( a decrease in the force of your urinary stream; nocturia (the need to pass urine frequently at night); post-micturition dribble (urine leakage on walking away from the toilet) .
Lifestyle measures to improve Lower Urinary Tract Symptoms:
Ideally you should have a daily fluid intake of 1.5 to 2 litres. Most which should be water or squash. A good habit is to drink a glass of water before going to bed, and on getting up in the morning.
Caffeinated beverages can act as bladder irritants. If you have symptoms of frequency and urgency, you should try caffeine-free products. Drink water or fruit squash instead of caffeinated drinks (tea, coffee, chocolate, Red Bull, Lucozade or cocoa). You should reduce your caffeine intake gradually (over a fortnight or so) to prevent withdrawal symptoms.
Large volumes of fluid over a short time, especially fizzy drinks, can cause rapid filling of your bladder, frequency and urgency. You should space your drinks evenly throughout the day.
Ideally, your urine should be a light straw colour (like champagne or white wine). Very dark or strong-smelling urine is too concentrated, and suggests you should drink more. If your urine is colourless, with no smell, you may be drinking too much. During hot weather, air travel, after exercising and during illness you need to drink more.
You should avoid going to the toilet “just in case” and do not strain to empty your bladder or bowels. Good habits to adopt are:
- allow your bladder time to empty properly – wait a few seconds, then try to empty more;
- do not drink before you go to bed – if you are troubled by getting up to pass urine at night; and
- only have a few sips of water at night – if you wake up needing a drink.
Bladder training:
Bladder training will probably help you by “re-educating” your bladder to hold a greater amount of urine.
It is used to treat frequency, urgency and urge incontinence due to an overactive or unstable bladder. Some people with these symptoms get into the habit of passing urine “just in case”, and the bladder can then “get used” to holding smaller volumes.
You must learn to control your bladder rather than allowing it to control you. When you feel the urge to pass urine, tell yourself that you are not going to go. Try to distract yourself for five to 15 minutes (use whatever method works best for you). If you do this every time you want to pass urine, you should find, after a week or so, that your urgency reduces.
The following week, do the same thing but now delay passing urine by a further five to 15 minutes. Your bladder will gradually learn to hold more, and your symptoms will slowly improve. Be persistent and remember that your bladder, like any other muscle in the body, may need several months’ of re-training to reach its full potential.
Pelvic floor muscle training:
- pelvic floor exercises can also help reduce urgency. Sitting or standing still when you get the urge, this will also help you concentrate on tightening your pelvic floor muscles.
The pelvic floor has several functions:- it supports your pelvic organs and abdominal contents – especially when you are standing or exercising;
- it supports your bladder to help stop leakage – sometimes the muscles need to work gently and sometimes (such as when you cough, sneeze or strain) they must work harder – if they are not working effectively, you may suffer from urinary incontinence; and
- it controls wind and allows you to “hold on” with your bowels.The sphincter (valve) muscles which close your bladder neck can be damaged by prostate surgery. If this happens, your pelvic floor muscles become very important in maintaining continence. You can also contract your pelvic floor muscles after emptying your bladder to prevent post- micturition dribble.
Other aspects:
Avoid constipationUrinary symptoms are often worse if you get constipated. Because the bladder and bowel are close to each other, a full bowel can affect your bladder function.- Eat a balanced diet – include both soluble fibre (oats, barley, berries & fruit) and insoluble fibre (roughage such as wheat-based foods, cereal, vegetables & nuts)
- Eat regular meals
- Empty your bowel when you feel the need – delaying may lead to constipation
- Maintain a good fluid intake – 1.5 to 2 litres (three to four pints) per day is ideal Lose weight To reduce the load on your pelvic floor, aim for an acceptable weight for your height and build. Being overweight – having a body mass index (or BMI) over 29 – can make stress incontinence worse. There are many ways of losing weight and your GP can advise you on the best method for you. Avoid heavy lifting lifting puts an extra strain on the pelvic floor. If you do need to lift a heavy object, tighten your pelvic floor before you lift and hold it tight until you have released the load. Stop smoking Smokers are more likely to have troublesome urinary incontinence because of the strain that coughing puts on the pelvic floor.