All men have prostate. Half would develop a prostate enlargement in their fifties. Half of those will develop symptoms. Divide those by two, and the resultant number would represent those who need medical treatment. It goes on, with half of those in whom medical treatment fails, necessitating an intervention.
Treatment of Symptomatic Prostate Enlargement
Surgery has progressed in the past century, from open, to endoscopic, to laparoscopic and now the robotically performed operations.
To manage a benign prostate enlargement, and for the past few decades, transurethral resection (TURP) has always been the gold standard and the benchmark against which other modalities are compared to.
If you imagine a timeline for the evolution of benign prostate interventions, you’d see not infrequently, many have evolved across the decades, most of which disappeared for a variety of reasons; some from lack of producing similar ( let alone better!) results than the gold standard TURP, others failed due to inferior long term results. Others were simply non financially viable.
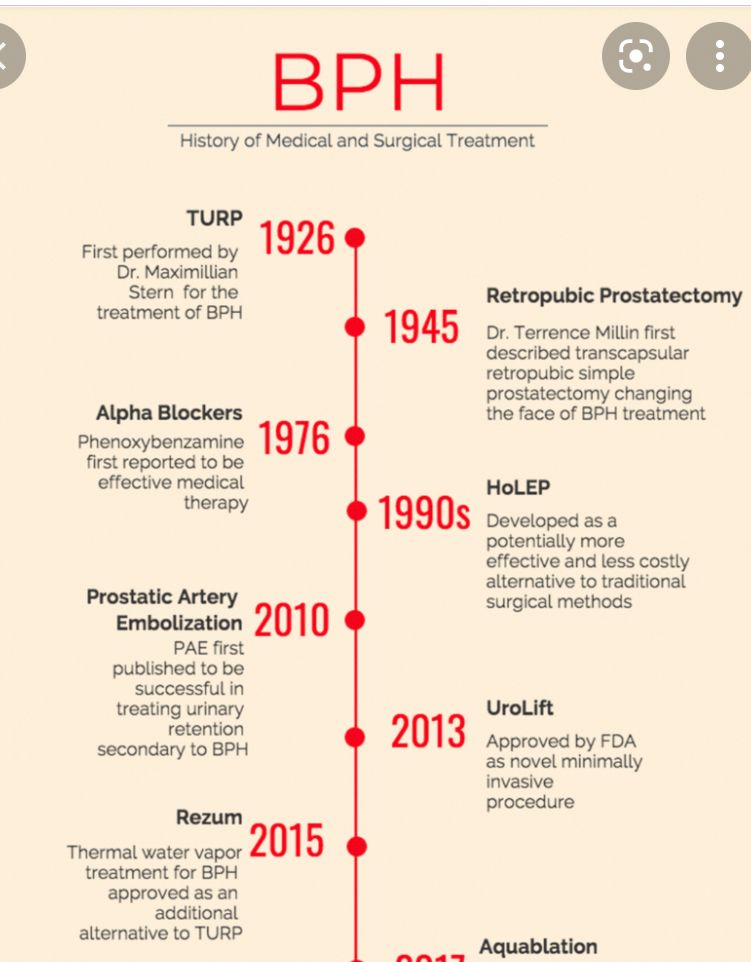
Some of the examples are the transurethral microwave thermotherapy (TUMT), transurethral needle ablation (TUNA), etc.
LASERs have entered this race, some as strong contenders, such as the Holmium laser (HOLEP, HOLERP), Greenlight laser ( stumbled initially but managed to pull through after enhancing its technology rendering better results). Thulium laser is another appealing technology.
Then came the vaporization (RESUM); it is a promising technology and it stands head and shoulder above the rest with its claims to preserve the ejaculatory function, being safe and bloodless. It can be carried out as a day case, which makes it very attractive in healthcare systems that struggle for hospital beds. The caveat is the severe storage symptoms that men suffer from in the first few days-weeks, during the shedding of the dead prostate tissues from the vaporization. Men would have to stay with a catheter for some time, which many, would find unacceptable.
However, for any problem, there is a potential solution. The EXIME short-term urethral stent would indeed sort out the severe storage symptoms ( in principle) by keeping the prostatic urethra patent during the sloughing period. However, while mechanically offering to keep the urethra patent, will it dampen the severe storage symptoms arising from the inflammatory response to the treatment? This needs to be prospectively assessed.
Last but indeed not least, is the UroLift. This one differs from all the other modalities (even including the gold standard) is the mere reliance on mechanically squeezing the prostatic lines thus creating a wider urethral channel for men to pass urine. No chipping, frying or freezing of any tissue, hence, one can assume that any inflammatory response ( if occurred after this procedure) should be trivial. It also preserves the ejaculatory function.
Now the challenges.. it is good for moderate-sized prostate and preferably with no median lobe. Other prostate sizes or shapes could impose a challenge.
It’s not cheap!
The learning curve is short, and its intermediate results are encouraging, awaiting long-term results. It per se does not preclude other modalities if it didn’t serve the purpose or if the symptoms recurred after some time.
Objective
In conclusion, there are several ways indeed “to skin the cat” none is perfect. One treatment can’t fit all conditions.
At the age of 51, and that’s my own personal opinion, if ( or should I say when!!) I need a prostate intervention, I’d probably go for the UroLift, knowing that it would, at least, buy me time until I’m less interested in preserving other functions, then I would go for other modalities ( possibly newer ones yet to be invented!).
Reference:
Soum Lokeshwar, David Valancy, Thiago, Fernandes Negris Lima, Ranjith Ramasamy. A Systematic Review of Reported Ejaculatory Dysfunction in Clinical Trials Evaluating Minimally Invasive Treatment Modalities for BPH. Current Urology Reports