The holy Ramadan season is upon us and we are devoted and hardcore dedicated for the long ritualistic fasting hours. To make this Ramadan season safe and healthy, urologist Dr. Ali Thwaini has a lot to share!
With long fasting hours, it is obvious that the water intake lowers to below the sufficiency levels and it is a major concern. Why?
With scorching sun, unbearable heat waves, and longer days, dehydration is a common issue accompanied by fatigue and weakness. This can ultimately lead to kidney stones and Urinary Tract Infections (UTI).
With dehydration clutching your body, dry skin and mouth, constipation, severe headache, thirst can be the resultant issues to resolve.
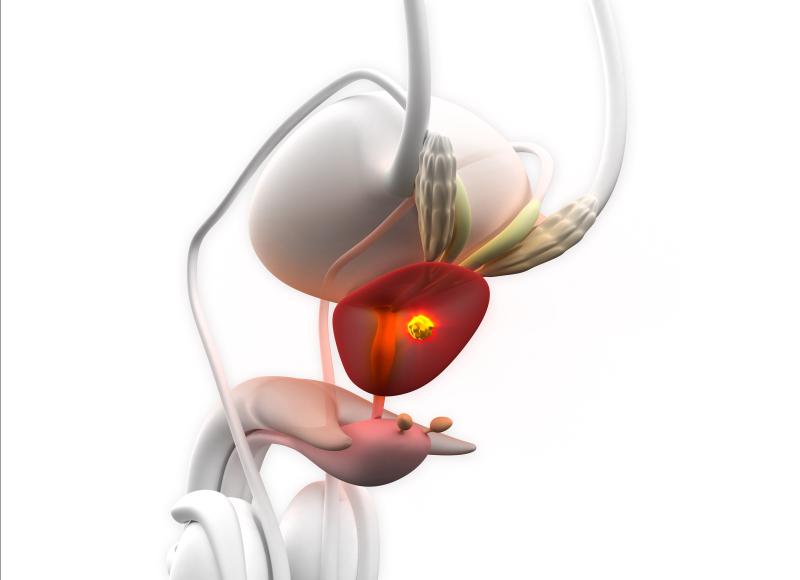
Kidney, Ureter or Bladder (KUB) stones and UTIs can arise in people who do not care to have at least 8 to 10 glasses of water a day. This is because, with no adequate intake of water, dilution of uric acid is not properly done and pH levels drastically reduce, leading to soaring acid levels and kidney stones start forming in your KUB.
UTIs tend to be a commonly sighted problem during fasting, especially in women.
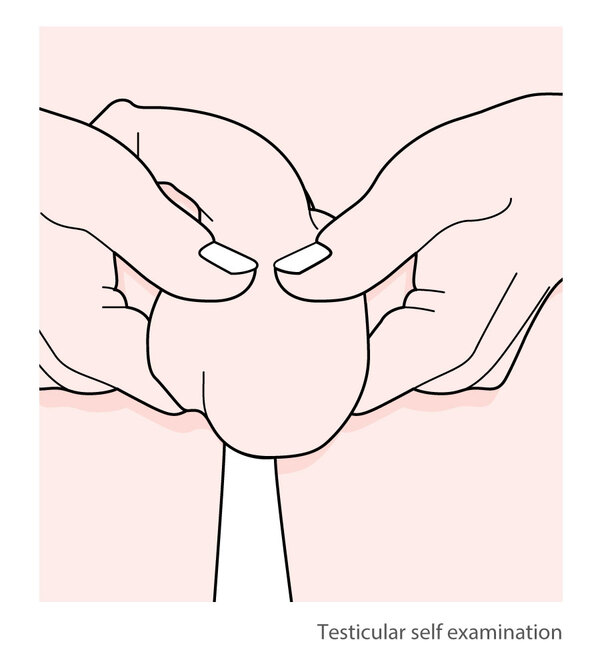
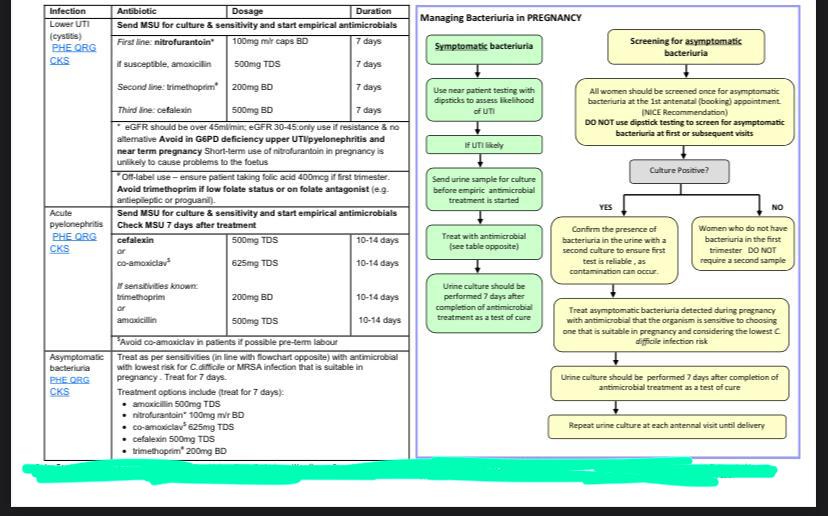
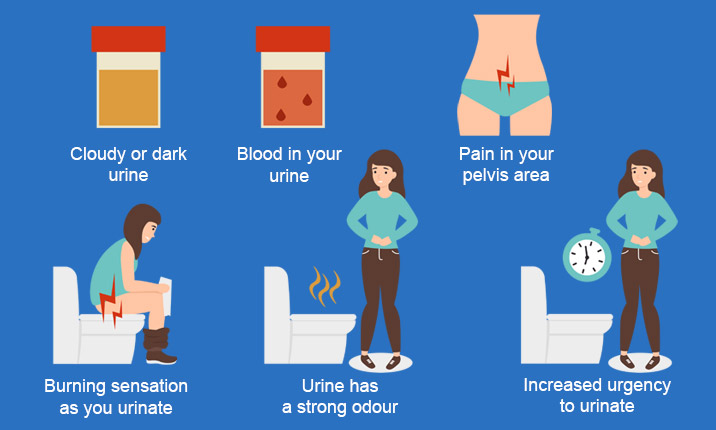
How do you find you are afflicted with UTI?
The initial symptoms of UTIs
- Having a burning sensation while urinating.
- Severe pain in the lower abdomen.
- Spotting blood in the urine.
- Lower back pain.
- Frequent urination accompanied by pain.
How UTIs affect your bladder can be put in simple words, it’s when there is an infestation of bacteria within the bladder. And this happens generally due to 2 main reasons:
- Reduced intake of water, hence the bacteria are not flushed out of the bladder and hence start infesting.
- Constipation can also result in the building up of bacteria which can resultantly affect one’s KUB.
It’s a major deduction that people with Diabetes are susceptible to bacterial, viral, and fungal diseases. Without proper medication, uncontrolled diabetes can result in chronic renal disease.
Quick remedies
- Take special concerns to stay highly hydrated during the nonfasting hours.
- Make sure to maintain good glycemic control with a proper diet plan and antidiabetic therapeutics.
- Drink at least 3 liters of water a day and stick to a low carb, low protein, and less salted diet
- Drink as much as fluids during Iftar and Suhoor in the form of fresh fruit juice to boost your immunity and nourish your body with a plethora of vitamins and minerals.
- Skip too many cups of coffee, since it’s an infamous diuretic and can dehydrate your entire system in the blink of an eye.
- Consume lime water with less added sugar, to boost the citrate levels of your body.
- Intake cranberry juice is also highly recommended to keep UTIs at bay.
With a proper diet plan and a hydrated body system, the majority of UTIs can be avoided to an extent. However, it’s wise to consult a urologist, for people affected by kidney disease, kidney stones, or UTIs before fasting to keep things safe and healthy!